|
|
|
Advance
care planning (ACP) is a key factor
in ensuring that your wishes and directives
are fulfilled, in terms of medical
and personal end-of-life care, as
well as death arrangements.
As the options available become more
complex in our modern-day world, it
is important to have your directives
written down — with copies given
to all who would be involved in your
medical treatment and final affairs.
This can be overwhelming,
so we encourage you to find someone
to guide you through the complexities. |
Summary
of Advance Care Planning for Final Affairs
On
this webpage, CINDEA provides a description
of the documents that may be required to
plan your end-of-life affairs. We
have attempted to answer some of the questions
you may have about Advance Directives and
Representation/Proxy Agreements, in particular,
which are perhaps the most important of
these documents as far as medical matters
go. In addition, we have provided
a brief checklist (at the
end of this page) of some of the
matters you may wish to consider as part
of your own advance-care planning. We
have attempted to answer some of the questions
you may have about Advance Directives and
Representation/Proxy Agreements, in particular,
which are perhaps the most important of
these documents as far as medical matters
go. In addition, we have provided
a brief checklist (at the
end of this page) of some of the
matters you may wish to consider as part
of your own advance-care planning.
This
page also includes a short overview of dementia
and how it is connected to advance planning.
Dying with dementia is becoming
increasingly common as people live longer,
since medical treatments have been found
for many other illnesses. The
modern-day phenomenon of dementia has many
issues associated with it that our culture
and our medical system have not yet resolved.
Nonetheless, dementia is a factor
that needs to be seriously considered during
the advance-planning process, as you may
not be able to make the necessary decisions
if you are affected by this condition in
the future later in life. |
|

Advance
Planning of Legal and Medical End-of-Life Affairs
Short
List of Final Affairs Documents
Please
note:
Some of these documents have different names,
depending on what province or territory you live
in. The particulars may also be somewhat
different, so please check on the specifics for
your area. The term 'Advance
Directive' will be used for all references to
advance health-care choices. The term
'Representation Agreement' (the term in BC) will be used for the
document that specifically designates the person
you have chosen to fulfill the Advance Directive,
or who will make medical decisions that it does
not cover. A Substitute Decision-Maker
may also be referred to as a (default)
Proxy.
Will:
Contains legal instructions on how to distribute
the assets in the estate after death; if there
is no will, the law determines distribution. Legal
will kits are available through various organizations
listed on our Resources
in Canada —
Pre-Death page. If you have multiple
assets, or your desires for their distribution
are complex (multiple recipients,
trusts, etc.), we advise that you consult
a lawyer who specializes in estate law.
(return
to top)

Power of Attorney:
A power of attorney (PoA) is used to delegate
financial and most legal decisions — but
generally not healthcare decisions —
to a person of your choice (usually
a friend or family member) while you are
alive. If you don't have a relative
or friends who can serve as power of attorney,
you can designate a respected professional such
as your lawyer, accountant or trust company —
but be aware that their services may be quite
expensive. After you die, all financial
and legal decisions are made by your executor,
not by the person who has your power of attorney
(unless they are the same person).
| There
are generally 4 kinds of PoA documents: |
| |
 |
|
general
or regular (not
commonly in use any more) |
 |
limited
(only a stop-gap measure when
travelling/etc.) |
 |
enduring/continuing
(in effect as soon as signed,
and continuing until it is revoked, or until
death) the most common form |
 |
springing
(so called because it springs
into effect in specific named circumstances
— usually when the person is no longer
fully capable of making their own decisions) |
(return
to top)

Expressed
Wishes/Personal-Care Wishes: "Expressed
wishes" is a term that refers to choices
— particularly for end-of-life care —
that are not specifically medical, but address
personalized 'quality of life' (frequently
referred to as "personal care").
| Expressed
wishes may include |
| |
 |
|
alternative
therapies |
| |
 |
nutrition
and hydration
needs and preferences |
| |
 |
safety
issues |
| |
 |
residence
and clothing
preferences (where possible) |
| |
 |
special
hygiene needs |
| |
 |
preferences
for recreation and
social activities (where possible) |
| |
 |
things
to do or not do to avoid discomfort
or annoyance |
| |
 |
personal
issues and anything of specific
concern to the person |
 |
spiritual-care
issues |
| —
as well as choices throughout the pan-death
process (pre-death care, active
dying stage, post-death care, funeral/memorial,
etc. See CINDEA's Post-Death
Care page). |
(return
to top)

Advance
Directive/Health Care Directive/Personal Directive/Power
of Attorney for Personal Care (or
Health Care) [Note:
this is sometimes referred to as a Living
Will, but that
I not a legal term in Canada except
in Nunavut]:
Details your wishes for medical treatment/care
if you are no longer able to make your own decisions
or communicate them (see below
for detailed description of Advance Directives).
 |
|
If
no Advance Directive exists, decisions on
treatment/care will be made by your Representative
or substitute decision maker. |
 |
|
The
default designation of who would be your substitute
decision maker is determined by a legal list,
with a specific ordering of blood/marriage
family members — and in some provinces/territories,
other people, such as closest friends. |
 |
|
If
no Representative or substitute decision maker
is available, decisions will be made by the
medical staff, based on normal practice (and
most often directed towards continuing life
-— the medical default position). |
(return
to top)

| Representation
Agreement (RA)/Health
Proxy (or
Agent) Agreement:
If no RA exists, and there is no appropriate
substitute decision maker, the courts will
appoint a legal guardian. Be
aware that whether either form of RA (below)
requires a lawyer may vary from one
province/territory to another. The
table below is drawn from the requirements
in B.C. as of the date this is written (October
2011). [Note:
If you are unclear about your needs, we advise
that you talk to a lawyer who specializes
in Elder Law.] |
| |
| |
 |
|
Standard
Agreement: designates person(s) who will
be your Representative/Health Proxy and make
decisions for non-life-threatening medical
conditions/circumstances, and possibly deal
with routine finances and personal care.
May not require a lawyer's signature.
[Note:
in some provinces/territories —
such as in B.C.
— it may
be possible for an adult to sign a standard
agreement after they are 'deemed incapable':
the focus is on 'degree of capability', rather
than a simple 'is or is not capable'.] |
 |
Enhanced
Agreement: designates person(s) to be
your Representative/Proxy for all medical
decisions, including those which are life-threatening.
If there is no such agreement,
and no substitute decision maker is available,
life may be extended beyond — and by
means against — the wishes of the patient
[Note:
a Standard RA does not automatically extend
to become an Enhanced one, if one's medical
situation becomes life-threatening.]
May require a lawyer's signature (as
of September 2011, this is no longer required
in B.C.). |
Please
note: much of the information on pre-planning
confuses the two issues of (a) what choices are
to be made, and (b) who will fulfill (or
make) them. For example, a
Personal Directive is commonly considered to be
the same as the older term for an Advance Directive
— 'living will' — but a Personal Directive
(such as the
one in Nova Scotia) includes a designation
as to who will make decisions for you when you
no longer can (similar to a Representation/Health
Proxy/Power of Attorney for Health Care Agreement). We
advise that you make a clear distinction between
(a) your written instructions/choices on health
care (the Advance Directive),
and (b) the written agreement as to who will fulfill
your Advance Directive choices and make all unforeseen
decisions (generally called the
Representative or Health Power of Attorney).
Part of the problem here is that there
is — as yet, but this seems to be changing
— no standardization of terms or legislation
in Canada.
(Return
to top)

|
Why
are Advance Directives and Representation/Health
Proxy Agreements Important?
In earlier generations, families tended
to live close by and to share traditions,
values, religion, and lifestyle choices.
The medical options were limited
— especially for terminal illness and
'extreme measures' treatments (which
has primarily developed since the 1970s).
People usually died before they
reached a prolonged state of severe dementia,
coma, or critical chronic illness.
As a result, family members usually knew
what each other's end-of-life wishes were,
and were available to fulfill them. |
|

Fire
—
remembrance flower mandala by Elli Boray
|
With
the medical and cultural changes of the 20th century,
end-of-life choices are no longer so straightforward. Family
members often live great distances from one another,
and may not be available when decisions need to
be made. Given divorce, re-marriage,
and/or common-law situations, there may be serious
questions as to who would be recognized as legitimate/legal
family (re the substitute decision maker list). Because of medical
advances (especially with chronic
illnesses) and increased longevity, close
family members (such as spouse
or siblings) — who would normally
make end-of-life decisions for each other —
may not be fully mentally or physically capable
of doing so. In our present global/multi-cultural
world, traditions have greatly diversified within
families, and the traditions themselves are changing
exponentially (as are the reasons
— such as ecological awareness — for
them doing so): as a result, family members
may hold very different values, or have very different
ways of expressing them. Some families
still are physically close and share traditions,
values, and lifestyle choices: however, in many
cases, it may be close friends — or members
of an intentional community one belongs to (faith,
etc.) — who are both willing, and
able, to fulfill one's end-of-life choices.
| This
modern situation also means that it is more
possible, and advantageous, to specifically
personalize our end-of-life choices —
both medically and otherwise (personal
care, post-death care and arrangements, etc.).
As cultural traditions change, there
is both a need to clarify our personal choices,
and the opportunity to do so, according to
our own values. As such, it is
necessary for all of us to discuss these matters
with our families, friends, and communities;
be very clear about what we want; and ensure
that reasonable arrangements are made to fulfill
our choices. However, "According
to a 2004 poll conducted by Ipsos-Reid on
behalf of the Canadian Hospice Palliative
Care Association and GlaxoSmithKline, 80%
of Canadians agreed that people should plan
for the end of life when they are healthy
– and yet 70% of them had not done so
themselves." (quote from
"How would you
answer these questions? " By Sharon
Baxter, Executive Director, Canadian Hospice
Palliative Care Association, Speak Up article)
[Note:
the March 2012 Ipsos-Reid
study, on the same issues, shows little difference
in the past 8 years.] |
|
"According
to the study, 65 percent of the doctors
(or former medical students) had created an advance directive,
i.e. a set of legal documents spelling out
in advance what sort of end-of-life care
they would like. Only about 20 percent
of the public does this. When
asked whether they would want .. CPR, if
they were in a chronic coma, about 90 percent
of the Johns Hopkins doctors said no. Only
about 25 percent of the public gives the
same answer."
From
article
"Doctors Really
Do Die Differently Research Says That More
Physicians Plan Ahead, Reject CPR, and Die
In Peace" —
based on John
Hopkins Precursors Study
—
by Ken Murray, MD, Clinical Assistant Professor
of Family Medicine at USC archived |
(return
to top)

Questions
and Answers about Advance Directives
1)
What is an Advance Directive?
An Advance Directive is a record of
your values and directives/choices — in terms
of general and/or specific medical care —
for when decisions need to be made about 'extreme
measures' treatment or terminal illness care.
It is only used if you become mentally
incapable or otherwise unable to communicate your
choices: until then, you retain the right to make
all medical choices for yourself. The
Advance Directive must be written and signed by witnesses while you are
still mentally capable — therefore, it is
important to do so before major medical problems
arise. It is your voice when/if you
can no longer communicate coherently or make considered
decisions.
| Please
note: |
|
a. |
|
In
some provinces/territories, it is not required
that Advance Directive choices be actually
written down. However, given
the complexities of both our modern world
and medical intervention — and especially
if you have specific or detailed choices —
we advise that your Advance Directive be both
written and witnessed. This
avoids any confusion or misinterpretation
if you are no longer able to communicate your
choices or make considered decisions, and
if the Advance Directive is required to determine
further treatment. In B.C.,
for example, a signed and witnessed Advance Directive has recently
become a legal written document, which must
be followed by medical staff if available.
However, to be legal, it
must be signed by 2 witnesses. |
| b. |
If
you have not addressed all major possibilities
in your Advance Directive — and one arises
— then decisions on treatment will be
made by your Representative/Proxy or substitute
decision maker. Therefore,
it is wise to use a comprehensive Advance
Directive template that brings up a wide variety
of possible issues that may arise — and
discuss them in detail with your Representative,
to give them some idea of what your wishes
might be in unforeseen circumstances. The
'table of contents' of the CINDEA-recommended
Advance Directive is available here
as a PDF download, but is not the entire AD
itself. |
| 2)
What is the value
of having an Advance Directive?
It ensures that your
values and directives/choices are known to
your medical practitioners, family and friends;
and are recorded clearly, to limit any bias
in their interpretation. An Advance
Directive is most important when family members
|
| |
|
|
 |
|
live
at a distance, |
 |
are
themselves not entirely mentally or emotionally
capable (or likely to be when
needed), |
| |
|
|
 |
|
do
not share the same values, or |
 |
are
not able to discuss end-of-life issues, |
| and/or
when the person's choices are very specific
(such as when to withhold or
withdraw life-support). |
| |
| Even
when this is not the case, Advance Directives
may remove much of the confusion that can
happen, as families struggle with unforeseen
medical decisions on behalf of the 'incapable'
member — as well as the potential guilt
for the decisions made, especially concerning
withholding or withdrawing life-support. |
|
Romayne
Gallagher, a physician, and founding director
of the division of palliative care at the
University of British Columbia. "Most
people find if they have some idea what their
loved one had in mind, it makes a difference."
.. research clearly shows that discussing
and planning your death means your wishes
are more likely to be followed. As
well, family members experience less anxiety
and depression in the aftermath, and report
that the process is less agonizing....When
families don't know the wishes of a loved
one, they almost always default to more aggressive
treatment - and often end up regretting the
decision, says Daren Heyland, an intensive
care physician.... (Quote
from the Globe and Mail 'end of life'
series, November 27, 2011 Why
are we afraid of talking about deat?
by Erin Anderssen) |
3)
Is having an Advance
Directive absolute assurance that your wishes/choices
will be followed? No
— because of unforeseen medical circumstances,
or new treatments available; or because the Advance
Directive may not be available in some emergency
situations. However, most palliative-care
or hospice organizations recommend having one
(and it may be required upon entry
into residential care); and as a result,
more medical staff are honouring them. If
it is not possible to follow the specific choices
of your Advance Directive, it will then be used
to understand your values and apply them to the
decisions that need to be made in that situation.
Please
note: although the use of Advance Directives
is growing, some medical practitioners are unfamiliar
with them, and may mistake them for a 'Do Not
Resuscitate' order — which is only one option
included in an Advance Directive, and one which
you may not have chosen. In any case,
it is wise to review your Advance Directive with
any doctor — or other medical staff —
primarily involved in your care, to ensure that
they understand your wishes if/when you are not
able to communicate for yourself.
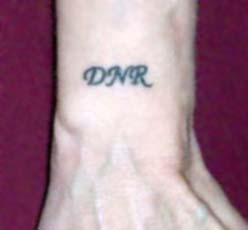
One
person's choice
The
only people in BC (and perhaps
other provinces/territories) who are
not required to abide by an Advance
Directive are paramedics — as it is not
likely that it would be immediately available
to them, in an emergency situation. However,
if they know there is a "No CPR/DNR"
order, they will not resuscitate.
The more usual ways of informing the paramedics
are a medical alert bracelet, a wallet card
(kept with the driver's licence),
or a "No CPR" order on the fridge
door (in a green casing).
One person has chosen the option
to tattoo it into her skin in locations that
the paramedics are unlikely to miss. |
|
 "No
CPR" tattooed
"No
CPR" tattooed
over her heart |
|
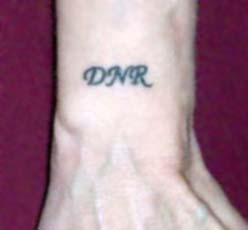 "DNR"
(Do Not Resuscitate)
"DNR"
(Do Not Resuscitate)
tattooed on right wrist, where paramedics
would look for a
medic alert bracelet |
4)
Is an Advance Directive
a legal document? Yes,
under common law — except for Nunavut, Nova
Scotia, New Brunswick and Quebec (which,
as of August 2011, have no legislation about Advance
Directives, or are in the process of changing
it) — although it does not have to
be signed by a lawyer. If you have
an Advance Directive, your Representative/Proxy
or substitute decision maker may be legally bound
to follow it (or advocate for it
with medical personnel). [Note: an Advance Directive has become a legal document
in itself, in B.C. It may also be
a legal document — under a different name
— in other provinces/territories.]
5)
What is the difference
between an Advance Directive and Expressed/Personal-Care
Wishes? An Advance
Directive contains instructions on medical care
—
including the withdrawal or withholding
of care to allow a natural death to occur.
An expressed wishes/personal care
document contains instructions or suggestions
on non-medical matters —
including personal care, vigils, memorials, where
you want to live, etc.
(return
to top)

Questions
and Answers about
Representation/Health Proxy
Agreements
6)
Who makes medical decisions
for you if you can't? Generally
there are two options — a Representative/Proxy
or a substitute decision maker. If
there is no Representative/Proxy, or the family
is arguing over who will make the decisions, then
the courts will appoint a legal guardian, which
can become a very lengthy and expensive process
— and the family or the estate will be charged
for the cost.
A
substitute decision maker is a default option
if there is no designated Representative/Proxy.
Each province or territory has a list,
in a prescribed order, of family members who can
act as substitute decision maker — generally
spouse, adult children (by age),
parent, sibling, and finally other family members
by birth or adoption (and in some
provinces, close friends). A
substitute decision maker will be chosen for you
(without your consent, if you are
not 'capable') if you have not designated
a Representative, and/or if your family does not
agree as to who will act as the substitute decision maker. [Note:
by law, a substitute decision maker cannot
be a family member who is in dispute with you
or has not had regular contact with you.]
7)
What is a Representation/Proxy
Agreement? It is
a document that designates your Representative(s)
and defines their responsibilities. There
are two types — and unless you are comfortable
with the default substitute decision maker that
would be chosen for you, it is wise to choose
the second type.
| a. |
|
Standard
Health and Personal Care Powers — which
only deals with 'personal care' and minor
medical decisions (as well
as, possibly, regular finances — bills
and bank accounts), and does not cover
major medical decisions. This option
is often used for disabled people who may
not be able to make informed decisions for
themselves. |
| b. |
|
'Enhanced'
or 'Additional' Powers — which does include
the right to make major medical decisions
(such as withholding or withdrawing
life-support), in addition to the medical
decisions covered by the standard agreement,
but generally does not cover finances. |
Please
note:
both these kinds of agreements may have different
names and/or conditions in your province/territory.
See our Resources
in Canada Pre-death page section on Advanced Care
Planning Resources for specific information
in your area.
8) What
is a Representative/Proxy/Health Agent?
This is someone who is specifically
designated by you, in a legally written and witnessed
document, to make medical decisions for you when
you can't (although they may also
support you while you still can); and who
is legally bound to advocate for the choices in
your Advance Directive, if one exists. This
may be a family member (should
you wish to designate someone who is not the first
on the substitute decision maker list)
or a close friend. A Representative
should be chosen in any situation where you have
concerns about the ability of particular family
members to understand and/or follow your choices
(whether or not you have an Advance
Directive), or when there are no family
members available to take this role.
It
is wise to name at least a primary and an alternate
Representative (or co-Representatives,
but define how they make collaborative choices)
— if not a 'default Representative' as well
(which can be a faith community). The
default Representative will be called on to act
in case of unforeseen circumstances where your
primary and alternate Representatives cannot serve.
It is recommended that the Representatives
NOT be the same as your power of attorney (who
deals with financial and legal decisions while
you are still alive —
i.e. not your executor, although you might name
the same person to hold both roles of PoA and
executor). It is also recommended
that the Representation Agreement NOT include
regular financial/legal duties, unless your financial/legal
matters are very simple and minimal (usually
only included in a standard Representation Agreement).
[Note: in BC at least,
a Representative can not be paid because of conflict
of interest issues, whereas a Power of Attorney
can be.]
9)
Does a Representation/Proxy
Agreement need to be signed by a lawyer? In
B.C., a 'Standard Health and Personal Care Powers'
Representation Agreement does NOT need to be signed
by a lawyer — and as of September 2011, an
'Enhanced or Additional Powers' RA also need not
be signed by a lawyer. You will need
to check the laws for your own province/territory,
as these may vary (check our Resources
in Canada Pre-death page, the section on
Advanced Care Planning Resources).
10)
Which has more power
— an Advance Directive or a Representation/Proxy
Agreement? Ultimately,
your Representation/Proxy Agreement will have
more power — due to the possibility of needing
to making decisions that are not addressed in
the Advance Directive, unforeseen medical options
that become available, or if a situation arises
where your wishes simply cannot be fulfilled. However, if the Advance Directive
is considered a legal document in itself, it will
have at least equal power to a Representation/Proxy
Agreement; and in many provinces, is equal to
your own voice (i.e. more powerful
than the Representation Agreement)
Many
Enhanced Representation/Proxy Agreement templates
give unlimited decision-making power to the Representative/Proxy
and do not address the presence of an Advance
Directive (even if the Representative
is legally bound by it). Although
none of us would like to think of a family member
or friend misusing this power, elder abuse is
a growing problem. [Note:
if you have any concerns about elder abuse, please
see our Resources in Canada Pre-death Page, section
on Elder
Law and Mediation CANADA.]
It is also possible that if your Advance Directive
is not comprehensive and/or discussed thoroughly
with your Representative/Proxy, they may misunderstand
your wishes. Therefore,
it is wise to ensure that your Representation/Proxy
Agreement clearly defines the role as following/advocating-for
your Advance Directive — as this will give
more weight and clarity to your Advance Directive
with your medical practitioners.
As an example, the Representation Agreement recommended
by CINDEA includes the words, "…in
accordance with my Advance Directive and expressed
wishes… whenever and in all matters possible."
(Return
to top)

|
Dementia
and Advance Planning
Dementia,
in particular, is a growing phenomenon.
Certainly, in earlier times, what was originally
called "senility" was not uncommon;
but because people didn't tend to live as
long, the condition did not become
as extensive as it is now. The
Alzheimer Society of Canada — in their
recent study Rising
Tide: the Impact of Dementia on Canadian
Society — predicts that there
are likely to be about 2.5 times as many
cases of dementia by 2038 as in 2011,
with the cost of care increasing 10 times
within a generation. Other studies
show that, "Of
those with dementia, 60% live in developing
countries, with this number rising to 71%
by 2040." [Quote
from Randall Parker's Future Pundit blog
on Total
World Dementia.]
Furthermore, 1
in 3 Seniors Dies With Alzheimer's or Other
Dementia |
|

Air
— remembrance flower mandala by Elli
Boray
|
Except
perhaps in the later stages, it is quite possible
for people with dementia to make decisions —
but it becomes progressively difficult (from
early stages on) for them to understand
both the context of the decision and its consequences.
There is simply not enough memory or cognitive
power, and decisions tend to be made on
immediate emotional reactions (for
example, refusing to take a bath, without any
understanding of the personal repercussions to
one's health).
| An
Advance Directive, for a person with dementia,
can be both a blessing and a curse.
It can be written in the very early
stages of dementia (when it
is only short-term memory that is being primarily
affected) — but not afterwards,
as it becomes less possible for them to consider
the ramifications of the possible choices.
Unfortunately, in later stages of dementia,
the person may have no memory of writing it,
and is likely to state immediate wishes that
are directly contrary to it. However
— especially if the Advance Directive
includes dementia provisions (a
statement of wishes, should the writer move
into dementia, and according to different
stages of the disease) — their
Representative/Proxy or substitute decision maker will have the guidance of their 'written
voice' as to what major medical decisions
to make, according to their considered choices
when fully mentally capable. |
|
Dementia is a progressive
disease, often described as a journey along
a winding pathway.
| |
Quote
from On the journey,
from the Dementia
Journey website (which
no longer exists, but the Alzheimer
Society of B.C. carries most of
its information). |
|
Dementia
is a very difficult disease to handle — both
for the person with dementia and their carers
(professionals and family/friends)
— as the person's personality changes considerably,
and sometimes becomes unrecognizable or the extreme
of earlier traits. If the Advance
Directive also includes a thorough review of personal-care
preferences, this can help in understanding immediate/emotionally-based
wishes; and may avoid unnecessary negative reactions,
that might eventually lead to a breakdown in care
giving — such as not being able to keep them
at home any longer. For example, a
simple note in the expressed wishes — "I
don't like yellow" — may explain
the resistance to wearing a certain piece of clothing.
A
comprehensive Advance Directive and Representation/Proxy
Agreement is, perhaps, the only way that a person
with dementia's own voice — their considered
choices — remains in place, able to guide
the very difficult responsibility of making specific
choices for them in a particular time/situation,
especially when it comes to major end-of-life
decisions.
[See also the Dementia Resources section on the
Resources
in Canada — Pre-Death page.]
(Return
to top)

Advance
Planning
for
the Pan-Death Process |
|

Summer — remembrance
flower mandala by Elli Boray
|
| |
| The
options for alternative medical care, personal
care, the pre-/during/post-death stages, and
burial/cremation are expanding, as |
| |
 |
|
our
culture becomes more multi-cultural (whether
ethnic or lifestyle variations); |
 |
medical
options are constantly being updated and/or
added; |
 |
natural/ecological
alternatives are considered; and |
 |
personal
values change. |
| |
| However,
at the end of life, it may not be possible
to thoroughly evaluate all of these options.
The Death Journeyer no longer has the same
energy to consider options, or may be incapable
of doing so. Also, the family
or carer(s) need to focus entirely on care
giving, plus other drains on their energy
and time, such as: |
| |
 |
anticipatory,
ambiguous and/or disenfranchized grief; |
| |
 |
financial
worries; |
| |
 |
dissention
in the family over who should be giving the
care and what the care should be; |
| |
 |
simple
exhaustion, especially after a long period
of caregiving; plus |
| |
 |
upcoming
legal concerns over wills, etc. |
Therefore,
we strongly encourage people to research and consider
their choices, while they are still reasonably
healthy and well in advance of any serious medical
condition (accident, stroke, etc.)
or the worsening of a chronic condition,
which may then become life-threatening. Remember:
any of us — no matter what our age —
could have an accident or a sudden illness, that
would compromise our ability to communicate our
wishes.
The
variety of matters to consider is described on
various pages on this site, but below is a quick
review of them. Some of these may
not be relevant to a particular person. However,
for all those that are relevant, it is important
to discuss them with the family/friends well beforehand,
so that they are familiar with the choices you
wish to make.
(Return to top)

Options
to Consider
| Senior/end-of-life/Advance
Planning consultants |
These
practitioners can help you navigate the options,
understand their consequences, and create
a comprehensive plan. See CINDEA's
Resources pages — Pre-death,
Post-death,
and Resources
Elsewhere (outside of Canada)
— especially the Death
Midwifery and related services and EOL
Advance Planning resources sections. |
| Hospice/palliative
care |
We
recommend you look at these two sites and
consider the issues they bring up.
 |
|
Canadian
Hospice Palliative Care Association
(which includes a directory
of Provincial Hospice/Palliative Care
organizations, under "Provinces") |
 |
|
Canadian
Virtual Hospice (a
wide variety of information on end-of-life
concerns, and information on Advance
Planning in each province/territory
under "For Professionals",
then "Tools for Practice",
then "Advanced care planning
/ Decision making", which has
7 pages of material —
a huge resource) |
| |
Support
from death doula or pan-death guide, palliative-care
teams and hospice volunteers, etc., on life
stories or legacy projects, 'self-aware
dying' support, appropriate visitation,
alternative therapies for comfort care,
family or professional caregiving support,
anticipatory grief, etc. |
| Pre-death |
Support
from a death midwifery practitioner, death doula, home
funeral guide, funeral celebrant, or clergy
on initial plans for the funeral or memorial
service — with the Death Journeyer being
directly involved if they so choose. |
| Dementia |
It
is very important to have some sort of dementia
provision in the Advance Directive;, and
to have a Representative or a substitute decision maker who will be capable of making
decisions based on your values, in case
of dementia. |
| During
dying/death |
Death
vigils or other forms of religious/spiritual
support (including living/pre-death
'Celebrations of Life'); bedside
singing; aromatherapy; attention
to mouth care (ice chips/ointment)
because the mouth becomes dry and painful
at this time; holding the Death Journeyer's
hands and/or gently stroking their head and
perhaps other parts of the body; any
other care that might contribute to physical
or emotional comfort during the dying experience. |
| Immediately
post-death |
Organ
donation; funeral-home services; family-based/at-home
post-death care (support from
death midwives or home funeral guides for
a home funeral); lying-in-honour
or wakes |
| Funeral
choices |
Traditional
burial; green burial; hybrid burial
(partially green); cremation; plus newer, more ecological
options to cremation — promession/cryomation
(freeze-drying — not available
in Canada yet); resomation/aquafication
(use of water, heat, and lye
to reduce the body to an organic residue —
soon to be available in Toronto and perhaps
elsewhere —
see our Resources in Canada page, section
on Additional
Natural/Green-Friendly Options for the Remains)
or Recomposition (composting
of bodies, not available in Canada as yet) |
| Final
ceremonies |
Funeral
service; service at graveside or before cremation;
memorial; obituary; on-line memorial/guestbook. |
|